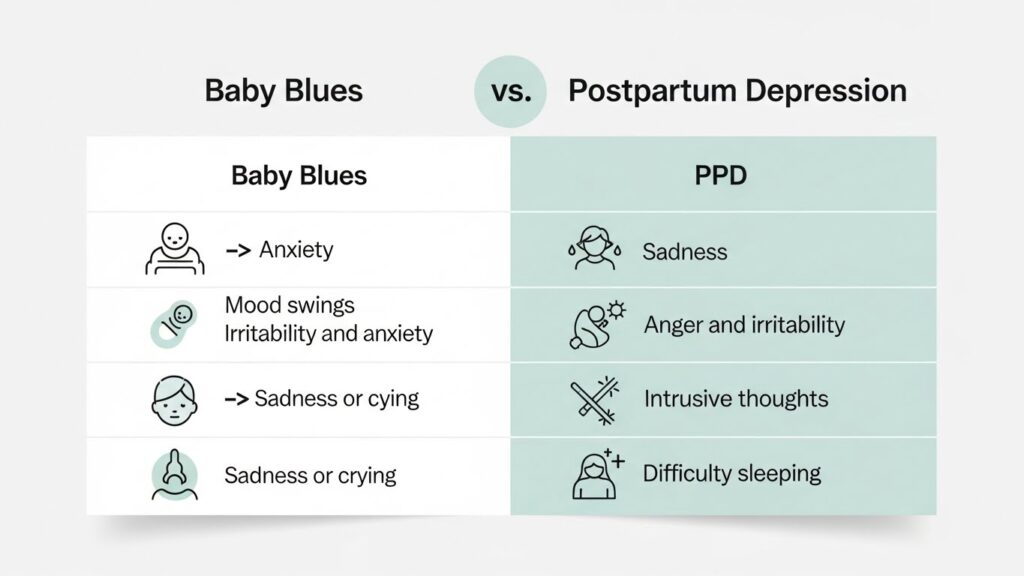
Postpartum depression (PPD) is a serious but treatable medical condition involving feelings of extreme sadness, anxiety, and exhaustion that can interfere with a parent’s ability to care for themselves or their newborn. Unlike the temporary “baby blues,” PPD is a clinical perinatal mood disorder that requires professional support. Postpartum depression is diagnosed when depressive symptoms last longer than two weeks after childbirth and involve a persistent low mood, loss of interest in activities, or intrusive thoughts that disrupt daily functioning.
This guide provides the clinical clarity and actionable steps necessary for a full recovery.
The Biological and Psychological Causes of PPD
As a perinatal specialist, I often explain to my clients that PPD is not a character flaw; it is a complex biological event.
The Hormonal Shift
Immediately after delivery, a person experiences the most significant hormonal shift in the human body. Estrogen and progesterone levels drop precipitously, which can trigger chemical changes in the brain that lead to mood swings and depression.
Sleep Deprivation and Circadian Disruption
The profound sleep deprivation associated with newborn care isn’t just tiring, it’s neurochemically disruptive. Lack of REM sleep affects the amygdala’s ability to regulate emotions, making a “hormone crash” feel significantly more intense.
Psychosocial Stressors
External factors such as a traumatic birth experience, lack of a social support network, or financial instability act as catalysts, increasing the risk of a Perinatal Mood and Anxiety Disorder (PMAD).
How to Get Help: Diagnosing Postpartum Depression
If you suspect you are experiencing more than just the “standard” adjustment to parenthood, the first step is a clinical screening. Identifying your symptoms through validated tools ensures you get the specific type of care you need.
The EPDS: Your First Tool for Clarity
The Edinburgh Postnatal Depression Scale (EPDS) is the “gold standard” 10-question screening tool used by therapists and doctors worldwide.
- What it does: It measures how you’ve felt over the past seven days.
- How to use it: Many providers offer this scale as an initial self-check. A score of 10 or higher is generally the threshold that suggests you should reach out to a perinatal mental health specialist for a formal clinical interview.
Finding Your Specialist: Differential Diagnosis
When searching for a therapist, it is vital to find a provider who can perform a Differential Diagnosis. This means they specialize in distinguishing between different perinatal mood disorders to create a targeted treatment plan. Understanding these differences helps you describe your experience more accurately during your first session:
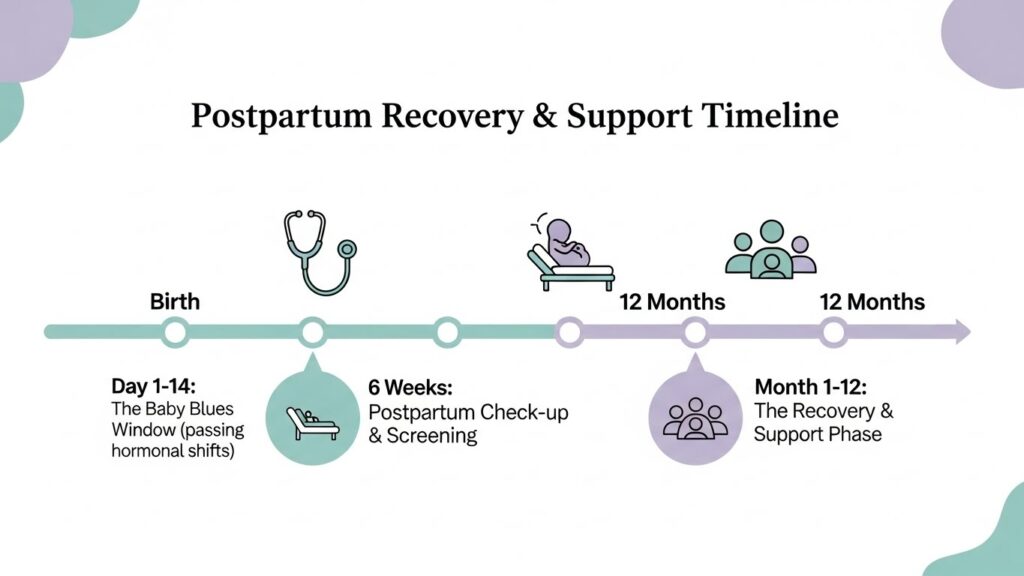
- Baby Blues: Often a physiological “hormone crash” affecting 80% of parents. If your symptoms resolve within 14 days, your provider may focus on rest and social support.
- Postpartum Anxiety (PPA): If your primary struggle is hypervigilance, racing thoughts, or physical symptoms like heart palpitations, you may need a therapist specializing in anxiety-reduction techniques.
- Postpartum Psychosis: This is a rare psychiatric emergency involving delusions or hallucinations. If you experience these, seek immediate emergency care at a hospital.
Evidence-Based Treatment Options
The “Gold Standard” for recovery involves a multi-modal approach.
Treatment Modality | Primary Goal | Clinical Focus |
Cognitive Behavioral Therapy (CBT) | Thought Reframing | Identifying and challenging intrusive thoughts and maternal guilt. |
Interpersonal Psychotherapy (IPT) | Social Support | Improving communication and navigating role transitions. |
Pharmacotherapy | Neurochemical Balance | Use of lactation-safe SSRIs or specialized meds like Brexanolone. |
Actionable Coping Steps for Immediate Relief
While therapy is essential, these daily protocols can help stabilize your mood during treatment.
- The “Rule of Three”: Prioritize 3 hours of consecutive sleep, 3 nutritious snacks, and 3 minutes of mindful breathing daily.
- Map Your Support: Create a “Support Map” identifying one person for childcare, one for household tasks, and one for emotional venting.
- Address Intrusive Thoughts: Understand that “scary thoughts” are often a symptom of anxiety, not a reflection of your character or safety as a parent.
Clinical Perspective
In my 3 years of practice, I recall a client, who felt she was “failing” because she couldn’t stop crying three weeks after birth. Once we identified her symptoms not as a personal failure, but as a biological response to an extreme estrogen drop, she felt empowered to engage in CBT. Within six weeks of targeted therapy and a stabilized sleep plan, she reported feeling like “herself” again.
References
- National Institute of Mental Health (NIMH): Perinatal Depression Facts and Statistics.
- Postpartum Support International (PSI): Standard of Care for PMADs.
- American College of Obstetricians and Gynecologists (ACOG): Screening for Perinatal Depression.




8 Responses