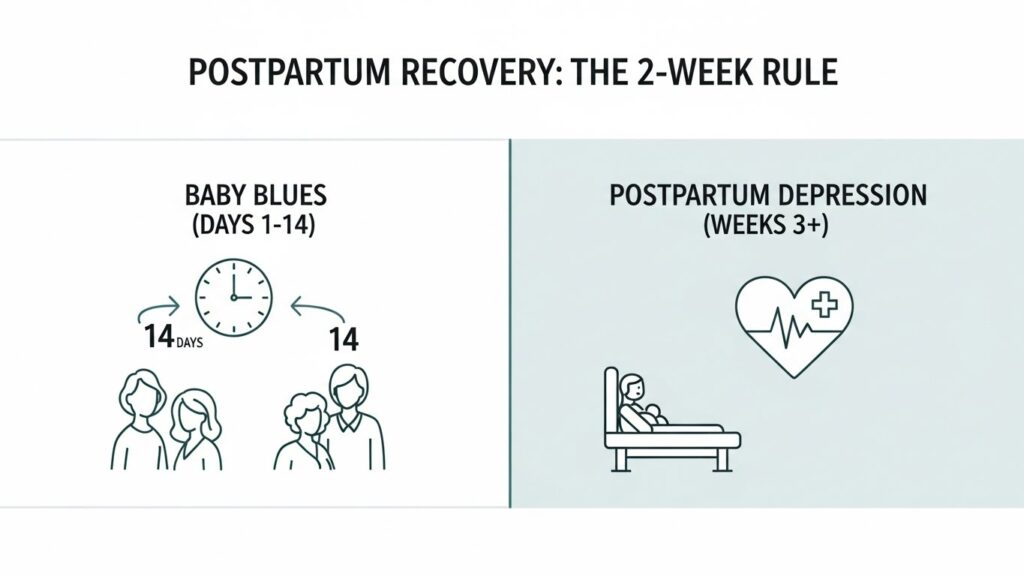
Bringing home a new baby is a profound life transition that triggers a whirlwind of emotions. While many new parents experience the “baby blues,” some face the more persistent challenge of postpartum depression (PPD). The primary difference between the baby blues and PPD is duration and severity: the baby blues typically resolve within two weeks without treatment, while PPD is a clinical disorder that lasts longer, feels more intense, and requires professional support. As discussed in our complete guide to postpartum clinical resource, identifying these distinctions is the first step toward securing the health of both you and your infant.
What are the “Baby Blues”?
The baby blues (maternity blues) are a mild, transient psychological condition affecting up to 80% of new mothers. They typically begin 2–3 days after delivery as the body undergoes a rapid estrogen and progesterone drop. Symptoms often include brief crying spells, irritability, and feeling overwhelmed, but they do not interfere with your ability to care for your baby.
What is Postpartum Depression (PPD)?
PPD is a more severe affective disorder classified by the DSM-5 as “depressive disorder with peripartum onset.” It affects roughly 1 in 8 women and, unlike the blues, can start anytime within the first year of birth.
5 Critical Differences to Watch For
1. Timeline and Duration
The baby blues follow a very specific “2-week rule.” They peak around the third to fifth day and vanish by day 14. PPD symptoms last significantly longer and will often worsen without clinical intervention.
2. Impact on Daily Functioning
If you have the baby blues, you may feel weepy, but you can still handle daily tasks like feeding or bathing. With PPD, the “functional compromise” is significant, parents may feel unable to get out of bed, handle household chores, or focus on their own hygiene.
3. Intensity of Mood and “Numbness”
While the blues are characterized by “emotional ups and downs,” PPD often presents as a persistent low mood or a feeling of being “emotionally numb” or “robotic.” This can lead to difficulties in maternal-infant bonding.
4. Presence of Intrusive Thoughts
A hallmark differentiator of PPD is the presence of intrusive thoughts, scary, repetitive, and unwanted thoughts about harm. While these are often a symptom of anxiety rather than intent, they are rarely seen in standard baby blues.
5. Treatment Requirements
The “Gold Standard” treatment for baby blues is rest, nutrition, and social support. PPD, however, typically requires Evidence-Based Treatment such as Psychotherapy (specifically CBT or IPT) and, in some cases, Pharmacotherapy (antidepressants).
Feature | Baby Blues | Postpartum Depression |
Onset | 2–3 days after birth | Anytime in the first year |
Duration | Lasts < 14 days | Lasts weeks, months, or longer |
Severity | Mild; self-limiting | Severe; debilitating |
Functional Impact | None to minimal | High; interferes with care |
Treatment | Support and rest | Therapy and/or medication |
When to Seek Help
As a Therapist, I advise parents to seek a screening if their symptoms:
- Do not fade after two weeks.
- Make it difficult to care for the baby.
- Include thoughts of self-harm or hurting the infant.
Clinical Insight
In my experience, many mothers dismiss PPD as “just being tired.” One patient waited six months to seek help, believing her inability to feel joy was a personal failure. Once we identified her symptoms as a clinical disorder rather than the “blues,” we began a treatment plan that restored her quality of life within weeks.
External Medical Sources
- Mayo Clinic: Postpartum Depression Symptoms and Causes.
- National Institute of Health (NIH): Perinatal Depression – StatPearls.
- Postpartum Support International (PSI): Standard of Care for PMADs.